Living with Nausea: My story in six charts
By Nicholas Rougeux, posted on January 12, 2025 in Data, Health
I used to have boring health. I never had more than the flu, been admitted to the hospital, and I could eat whatever I wanted, whenever I wanted. In late 2023, that changed when I developed chronic nausea.
The nausea started on November 20, 2023, with what I thought was nothing more than a mild upset stomach and has continued every day since, with varying intensity without any clear triggers. I’ve seen a dozen doctors, tried many medications, and have been subjected to more tests than before I became ill. Nothing pointed to a clear cause and no treatment has had lasting effects.
Chronic nausea is invisible and debilitating.
I’m learning how to be me again.
I never gave much thought to what I ate. I ate when I was hungry, enjoyed going to work, lost myself in my projects, and visited family regularly, eating out often on trips. Now, I carefully monitor everything I eat and have up to seven small meals a day. I’m only able to eat small amounts of food at a time because I feel extremely full if I have anything resembling a complete meal. I’ve learned to eat through the nausea. I rely on foods that are easy to digest and eat roughly every two hours so I can get enough nutrients to maintain a constant weight. I used to travel every year to visit family but have had to cancel more than a year’s worth of trips because there have been many times when I could barely leave my house to run errands, let alone fly to another state. I take frequent naps, not because I’m tired, but because they allow me to escape the awareness of how I feel. My life revolves around how poorly I’m feeling and it’s hard to focus on much else.
My doctors initially diagnosed me with gastroparesis, which means food didn’t pass through my stomach as fast as it should, and as a result, ferments and causes nausea. Later, that diagnosis was broadened to include functional dyspepsia and visceral hypersensitivity—both of which are vague umbrella terms that essentially mean I have an upset stomach with no clear cause and no cure.
When I realized the nausea was becoming chronic, I started doing one thing I could control—collect data about it. At the end of each day, I took up writing basic notes about how I felt that day, any treatments I tried, and assigning a number to it from 0 to 10 based on how nauseous I felt.
- No nausea all day
- Occasional periods with little or no nausea
- Noticeable but manageable nausea all day
- Steady nausea all day with difficulty focusing, one or two naps needed
- Unavoidable nausea with multiple naps needed for relief
- Constant strong nausea all day, multiple naps needed
- Strong nausea all day and schedule changes needed for relief
- Vomiting at least once, hospital visit optional
- Unable to keep food down, hospital visit needed
- Vomiting, pain, hospital visit
- Prolonged hospital visit
Originally, I tracked this to help my doctors better understand how I was feeling and create new treatment plans but that never happened, despite mentioning it to every doctor I’ve seen. Instead, I use it as a point of reference to remind myself what I’ve tried and to identify trends.
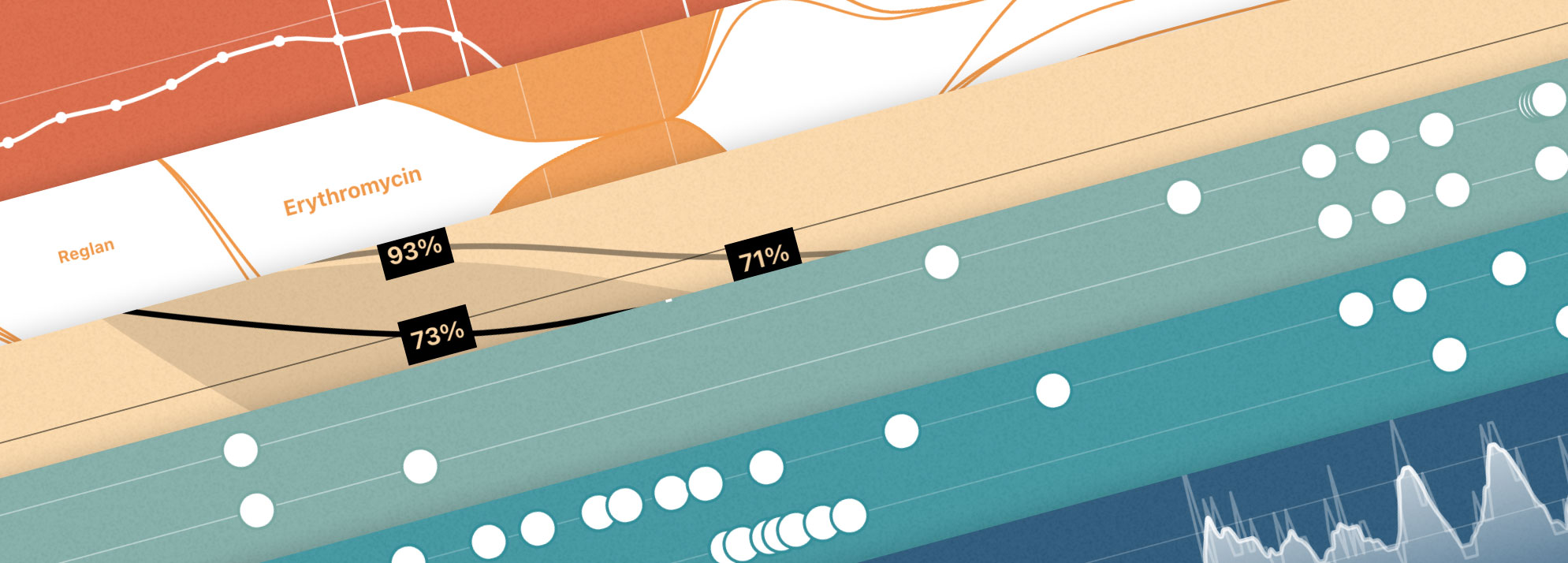
What I’ve found most interesting is the regular intervals at which my nausea flares up—about two weeks. This was surprising because I didn’t expect there to be such regularity. I’ve learned to consider this pattern when evaluating a treatment’s effectiveness. If a treatment had a meaningful impact beyond two weeks, it would be considered effective. Unfortunately, few have.
I’ve seen a range of doctors over dozens of visits in an effort to find relief, including my regular doctor, gastroenterologists, surgeons, therapists, a dietician, and a neurologist. The conversations I’ve had have typically been less than an hour long and comprised me giving a too-brief summary on how I’ve been feeling, reviewing tests results, some general questions about any changes in my habits, and a suggestion to try anti-anxiety medication, over-the-counter medication, or continue waiting to see if my symptoms improve on their own.
From November 2023 to May 2024, I saw my gastroenterologist, psychologist, and dietician on a regular basis. By summer, I started to feel better—even without medication—so appointments were scaled back. The nausea never completely subsided but felt manageable. However, it increased substantially toward the end of June, which prompted me to consider seeing other doctors to help me cope. I met with a neurologist, who was kind enough to listen to my story from beginning to end over the course of two hours. The outcome was similar but I was glad I had the chance to tell him my full story. I started seeing a psychiatrist to see if off-label use of psychiatric medication would help but as of this writing, I’m still evaluating its effectiveness.
On two separate occasions, doctors recommended trying gut-directed hypnotherapy. During the winter from December 2024 to February 2025, I decided to try it out since I felt I had tried so many other methods and I was fortunate enough that my insurance covered the cost. I attended seven virtual sessions over two months and listened to recordings each morning between appointments. The experience was pleasant and my therapist was nice to talk to and listen to. I experienced a decrease in nausea as the sessions went on but that also coincided with other medications I was taking so its effectiveness wasn’t definitive.
Appointments have been emotional roller coasters. Before each one, I naively started to hope that a recent test or experience with medication would reveal something new, or my doctor would have a new treatment to try. Often, the outcome is hearing that everything “looks normal” or that my problems are due to anxiety, which are two of the most crushing responses to hear, especially when I feel far from normal. Weeks or months have often separated appointments, partly because of availability, but also because trying new treatments takes time. Waiting months to see doctors or try treatments only to be told the same result after a short 30-minute visit is a constant source of frustration.
None of my doctors could identify a clear cause for the ongoing nausea but two key events may have contributed:
- On September 19, 2023, I tested positive for COVID-19. Having been vaccinated, it seemed to be a mild case with common symptoms—such as congestion, loss of smell, loss of taste, and of course, nausea. Unusual symptoms included vertigo and a numb toe. After 12 days, I felt normal again and had no lasting ill effects.
- On November 2, 2023, I caught the stomach flu and felt nauseous during the last day of a vacation in Florida and collapsed after standing up too quickly, hitting my head on the way down. I’ve always been somewhat prone to vasovagal syncope but only succumbed to it a handful of times. After coming to in less than a minute, I vomited and had a panic attack. The nausea subsided a few days later with no lasting ill effects. Doctors suspected it was little more than a stomach bug.
These two events were far enough away from my initial onset of chronic nausea that none of my doctors could definitively say if either was the cause of my nausea but believe they may have damaged some of my gastrointestinal nerves. Unfortunately, knowing a potential cause doesn’t necessarily result in an effective treatment.
Procedures I’ve had include numerous blood draws, CT scans, gastric emptying studies (GES), ultrasounds, and a failed pharmaceutical clinical trial. Early on, a lot of the standard tests were performed to rule out obvious causes like obstructions, cancer, etc.
The only test that showed something conclusive was my first gastric emptying study. Out of all the tests I’ve had, it was the most pleasant because it simply involved eating some scrambled eggs laced with a harmless radioactive tracer along with a piece of toast and taking scans of my abdomen over the course of four hours to see how the food moved through my system. After four hours, I should have had 10% or less in my stomach but in December 2023, I had 41% remaining, which indicated gastroparesis. Based on that, I was prescribed a few medications to make my gastrointestinal muscles work more efficiently but none had a lasting effect. The second study I had in September 2024 showed 8% remaining, at which point my gastroparesis was considered resolved but my symptoms persisted.
There was some concern early on that I may have median arcuate ligament syndrome (MALS) because one of my arteries appeared more compressed than expected in an ultrasound but that was ruled out after a follow-up ultrasound and a consultation with a vascular surgeon, who didn’t feel there was cause for concern.
ER visits bookended 2024—one in January for excess stomach acid caused by stopping an acid-blocking medication and again in November for a suspected small bowel obstruction, later thought to be enteritis. The latter required staying in the hospital for four days with an NG tube in my nose to drain my stomach (not a fun experience). My nausea subsided while the tube was in place but came back a couple days after being discharged. Despite the circumstances, the lack of nausea was a welcomed, albeit brief relief. During my hospital stay, my many tests were punctuated by panic attacks. Prior to becoming sick, I hadn’t had a panic attack but quickly learned what they feel like so I know what to expect in the future if I feel one coming on. The hospital staff were angels that provided immeasurable help throughout my stay in the hospital and I will be forever grateful for them.
I’ve tried numerous over-the-counter and prescription-strength medications since my nausea started with varying levels of success. Few medications had an immediate effect, so I often had to wait weeks to determine if they helped and they often came with side effects.
The earliest medications I tried were over-the-counter like Dramamine and FDgard but they did little to help and thankfully had no side effects. When those didn’t work, Zofran (often prescribed to cancer patients going through chemotherapy) was prescribed but only lasted a short while. Zofran did cause constipation so more medication was needed to keep that at bay.
Acid-reducing medication like omeprazole and pantoprazole were prescribed, thinking that my nausea was due to excess stomach acid, but they didn’t touch the nausea. I learned the hard way that stopping pantoprazole suddenly is not recommended because doing so caused excess acid and my first trip to the ER.
To help with motility, or the movement of food through the digestive tract, I tried Reglan for about two months. It had no positive impact on my nausea but did cause strong hunger pangs before meals, which implies it had some positive effect on motility. My muscles also started twitching occasionally, which could have been signs of early tardive dyskinesia (a common side effect). It can also become chronic and incurable if left untreated so once the twitching started, I discontinued it.
Erythromycin was prescribed toward the end of February and was the first medication with a noticeable positive effect and may have contributed to why I was able to spend about two months after my regimen without medication. It’s primary use is as an antibiotic but is used off-label to treat delayed gastric emptying (gastroparesis) and nausea in lower doses. The only negative side effect was a strong sense of hunger before meals. When my nausea started to increase at the end of June, I was prescribed a second round but it wasn’t as effective—a common experience for those taking it long term.
In August 2024, I learned of a clinical trial for Tradipitant—a new drug that was supposed to help reduce nausea in gastroparesis patients. I had to go through a screening period but made it into the trial and took it regularly for two months. Ultimately, the medication didn’t have any positive impact on my nausea but also didn’t cause negative side effects. While it was a lot of time to spend on an experimental treatment that didn’t pan out, I’m glad I did it. Otherwise, I would have forever wondered if it could have helped me.
Since September 2024, I’ve also been on increasing dosages of mirtazapine for depression and an off-label use of reducing nausea as well as Pepcid AC to keep stomach acid at bay. The side effects have been minimal and manageable. From December 2024 to March 2025, I tried Marinol—a synthetic form of cannabis to help with nausea, appetite, and fullness. Over the course of 80 days, I had a hard time telling if it had any measurable effect. There were periods of low nausea but nothing lasting. Even with insurance, it was prohibitively expensive and I often had to travel to pharmacies hours away to get prescriptions filled. As a result, I decided to taper it off per my doctor’s recommendation. Unfortunately, a week after I stopped entirely, I experienced the worst prolonged flare to date that lasted most of March—likely due to withdrawal.
Two over-the-counter medications have proven to be surprisingly effective: ginger and pectin lozenges. When my chronic nausea began, I wrote off ginger because I had tried Dramamine ginger chews with no success. Toward the end of December 2023, I bought several kinds of lozenges to give them another try and was pleasantly surprised to find that UpSpring Stomach Settles ginger lozenges helped when my nausea was mild and Halls Throat Soothing drops helped when I was feeling the effects of excess acid. Both helped within minutes and even though they only lasted a short while (hours at most), having them available has been a big help physically and mentally. Both are available on Amazon and Walgreens.
Throughout this ordeal, my weight has also been a constant focus. I’ve tracked my daily weight since August 2022 purely out of curiosity after seeing how others have tracked their weight and shared how it was affected by diets, medical conditions, life events, etc. I found it interesting to see how my weight fluctuated based on diet, exercise, travel, and even sleep. In an effort to keep it accurate, I developed the habit of weighing myself first thing in the morning and last thing at night and tracking the data using the Health app on iOS. This highlighted a problem that I was unaware of when my chronic nausea first started: I stopped eating enough.
When I was nauseous, the last thing I wanted to do was eat so I simply ate less in a futile effort to keep it at bay. As a result, I started shedding pounds and not in a healthy way. Looking back to before I caught COVID, my weight hovered just below 170 lbs. and my height was 5′9″. I lost some weight during COVID then it fell off sharply once the chronic nausea started. At my lowest in March, I weighed about 146 lbs. I struggled a great deal to find foods with enough calories and nutrients to maintain a healthy weight. My sessions with my dietician helped me figure out what I could eat and get me back on track. Over the next several months, I slowly inched back up to about 161 lbs. by June. Unfortunately, the increasing nausea around that time and subsequent hospital stay in November resulted in more weight loss, but I am slowly doing my best to gain it back.
A few of my doctors have recommended that I stop tracking all this data to improve my mental health and stop focusing on how I feel. While I understand why, I continue because I won’t be able to remember everything and I still hold out hope of finding meaningful information in all the noise. If nothing else, my experiences may prove useful for others going through similar situations. For better or worse, it’s become a cornerstone of my illness.
The hardest thing to come to terms with is that I likely won’t get better. There’s always the chance that my chronic nausea could go away on its own but that uncertainty is daunting. My family and friends have been invaluable in helping me through this long chaos. I love them more than they could ever know. There are more options I can try and I intend to try everything I can until I find something that works.
I will do everything I can to make my health boring again.
Update March 1, 2025: The charts in this blog post have been updated with data from February 2025 and will continue to be updated monthly for the foreseeable future. A paragraph has also been added that describes my experience with gut-directed hypnotherapy.
Update April 1, 2025: A paragraph has been added that describes my experience with Marinol withdrawal.
Author’s notes
I am not a medical professional. This blog post does not constitute medical advice. The information in this post is about what I’ve tried as well as what has or hasn’t worked for me. Consult your doctor before making medical decisions.
This blog post was inspired by Giorgia Lupi’s excellent 1,374 Days of COVID, chronicling her life-changing experience living with long COVID.